MICROBIOME AND MICROBIOTA: WHAT IS THE DIFFERENCE?

The microbiota is the set of microorganisms living in a specific environment (called microbiome) in a host (here, humans). We can, therefore, define the microbiome more simply as a planet, and the microbiota as its inhabitants. According to Chen et.al (2013), the microbiome refers to the specific environment in which a microbiota evolves. The microbiome encompasses all environmental conditions, such as temperature, pH, hormones, lipid or protein richness and exposure or not to light and UV.
The microbiota includes different types of microorganisms: bacteria, yeasts, fungi and viruses. Within microorganisms, there are prokaryotes and eukaryotes. Prokaryotes are single-celled organisms without a nucleus, like bacteria. Of these, there are two types: Gram-positive or Gram-negative, depending on their ability to retain a specific dye. Eukaryotes are organisms made up of several cells and possessing a nucleus, like fungi. The diversity and number of microorganisms depends on the location and its environment. The activity of these microorganisms depends on the state of health, genotype, diet and hygiene of the individual.
SKIN MICROBIOTA : A FRAGILE BALANCE
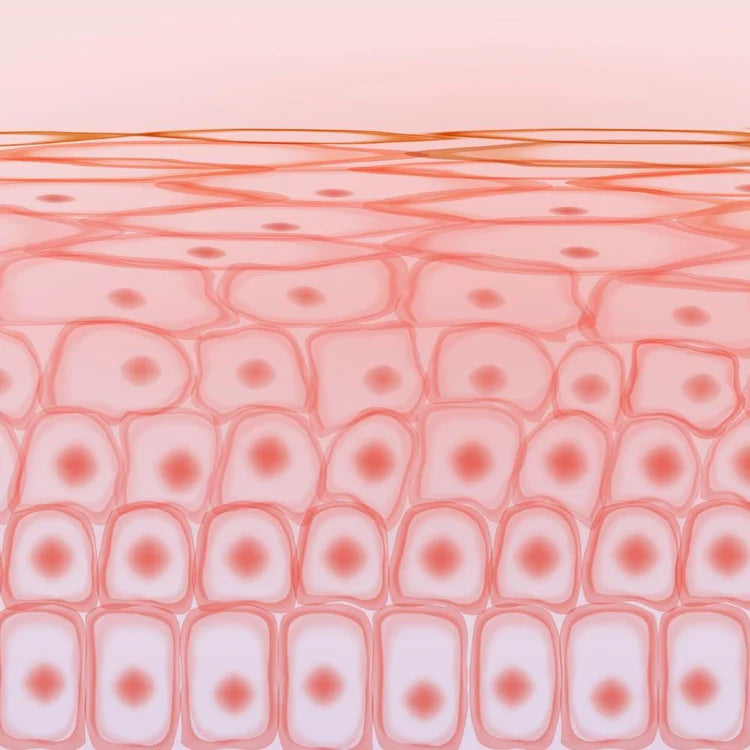
The skin is the interface with the external environment. As such, it is covered with a multitude of microorganisms: more than a million per cm² . The skin microbiota includes all the microorganisms that live on the surface of our skin. According to the Human Microbiome Project, it is distributed over the different layers of the skin, and can affect skin functions. The facial microbiota is mainly made up of bacteria but also of fungi and viruses.
The human body, and more specifically the immune system, manufactures anti-microbial peptides (like beta-defensin). They will prevent the proliferation of bad bacteria. But we also have good ones on the surface of our skin that help our immune system regulate the bad ones. It is important to conserve them and help them stay alive. It is also necessary to control the proliferation of bad ones, and prevent them from associating with each other (forming a biofilm), because that is where skin problems will appear. Pollution, stress and poor diet contribute to the imbalance of the skin microbiota.
COMPOSITION OF THE MICROBIOTA
From birth, the skin is colonized by microorganisms, and will be so throughout its life. Bacteria, fungi, viruses, parasites and mites are found on the skin. Bacteria are the best characterized microorganisms of the skin microbiota. The main ones are: Actinobacteria, Bacillota, Bacteroidetes and Pseudomonadota.
The skin microbiota is divided between a resident flora and a transient flora. The resident flora has a stable composition and distribution. It is composed of Gram-positive (Staphylococcus, Corynebacterium, Propionibacterium, Micrococcus, Brevibacterium), Gram-negative (Acinetobacter) bacteria, mites (Demodex), fungi (Malassezia) and viruses (human papillomaviruses). The Propionibacterium family of bacteria is most prevalent on the face, along with Propionibacterium acnes, which can trigger acne.
The transient flora is mainly made up of Saprophyte microorganisms. These are organisms that are non-infectious but can be colonized by organisms that cause certain diseases. These are Gram positive bacteria (Staphylococcus, Streptococcus, Bacillus, Neisseiria), Gram negative (Pseudomonas) and fungi (Candida).
BACTERIA: SURFACE LAYER OF THE SKIN
Staphylococci is the most represented family. The species S. epidermidis is the main species of the superficial layer of the skin (horny layer of the epidermis). The species S. aureus is generally considered to be pathogenic. However, it is present in the resident flora of the skin microbiota for 20 to 40% of the population.
Coryneforms are bacteria that draw lipids from the medium. They can survive in environments with high salt concentration. They are mainly found in the superficial layer of the skin, and in sebum-producing regions.
Propionic bacteria is the family of species Cutibacterium acnes, Propionibacterium avidum and Propionibacterium granulosum. These bacteria release fatty acids and allow their adherence and colonization. Cutibacterium acnes produces porphyrins in large quantities, which can help in the treatment of acne.
MUSHROOMS: FACE AND SCALP
The most common fungus on the skin is Malassezia. It is present in more than 90% of adults, its colonization starts after birth. Mushrooms are still much lower in number than bacteria, since it is 10 to 100 times less present than certain bacteria. The amount of Malassezia seems to be greater in men than in women, and it is more present in summer than in winter. These fungi are lipophilic, so they will prefer sebum-rich areas like the face and scalp. Among the Malassezia, we find Malassezia furfur, which can cause seborrheic dermatitis in particular. Mushrooms also contain Candida. These are pathogenic microorganisms, present in psoriasis or atopic dermatitis.
VIRUSES AND MITES
Viruses are cellular parasites: they need a host cell to reproduce. They can infect all types of cells and microorganisms. They do not necessarily cause disease in humans.
Dust mites are part of the animal kingdom. They are present in the follicles of the eyelashes and eyebrows. The mite species Demodex spp resides in the skin microbiota and the Demodex folliculorum species resides in the hair follicles.
A UNIQUE MICROBIOTA ACCORDING TO THE INDIVIDUAL AND THE LOCATION OF THE SKIN
The cutaneous microbiota presents a double diversity. We observe both a difference within the different areas of the body of the same individual, but also differences for the same area between several individuals. As microorganisms are specific to the environment in which they are found, 3 main areas of the skin have been defined: the dry area, the wet area and the sebaceous area. Each area hosts a unique skin microbiota. Its composition depends on several factors: environmental conditions (pH, humidity, temperature, sebum content), endogenous type (age, sex and genetics) and exogenous type (bacterial adherence, environment, hygiene and mode of life). This composition therefore evolves over time but seems to stabilize in adulthood.
The sebaceous zone has many sebaceous glands and has hairs. It is found on the forehead, head, neck, nostrils and back. It has the lowest diversity of bacteria, with mainly Actinobacteria. The dry area has a thick stratum corneum (surface layer of the skin), eccrine glands and lacks hair. It is found on the forearms, buttocks, hands and legs. This is the area that has the most families of bacteria, with mainly Proteobacteria. The moist area has lots of hairs and apocrine glands. It is found in the armpits, the folds of the elbows and knees, the heels and the scalp. It mainly presents Corynebacteria and Proteobacteria. Some species like C. acnes are particularly specific to an individual, while a species like S. epidermidis is more specific to an area of the human body.
ROLES OF THE CUTANEOUS MICROBIOTA
BARRIER FUNCTION OF THE SKIN
All the microorganisms that make up the skin microbiome help strengthen the skin's barrier function. The S.epidermidis bacteria activate a protein, allowing tight links between keratinocytes. The S.aurus bacterium converts an amino acid present in large quantities in the skin (histidine) into trans-urocanic acid. This contributes to the natural moisturizing factors of the skin and to the protection of UV rays. In addition, Corynebacterium spp has the ability to modify the lipids in its environment and therefore the composition of the sebum and the stratum corneum.
The skin microbiota also participates in the synthesis of antimicrobial peptides by the human body. Propionic bacteria are able to regulate pathogenic bacteria, fungi and viruses. We should also mention S. epidermidis, which is able to increase the diffusion by keratinocytes of antimicrobial substances.
PROTECTIVE ROLE
All the microorganisms of the skin microbiota play a role in protecting the skin. The presence of a resident microbiota makes it possible to limit infections by a phenomenon of competition. Indeed, the growth of pathogens on the surface of the skin is reduced, due to competition for nutrients and for space.
Microorganisms are also able to modulate their environment. For example, some can modify the pH and create an unfavorable environment for pathogens, or P.acnes, which is able to acidify the skin and thus reduce the presence of Streptococcus pyogenes and S. aureus. In addition, some microorganisms are able to produce anti-microbial factors. Let's mention Staphylococcus epidermidis, which produces antibacterial molecules, capable of reinforcing the role of anti-microbial peptides produced by the immune system and allowing the fight against skin pathogens.
Certain microorganisms are also capable of inhibiting the formation of biofilm, that is to say the association and attachment of bad bacteria to each other and to the skin. S.epidermis is capable, for example, of inhibiting the biofilm of S.aureus.
ROLE IN IMMUNITY
The microorganisms of the microbiota would also play a role in immunity, and therefore in our health. They develop the immune system and regulate inflammation. For example, S.epidermidis allows the functioning of the cutaneous immune system, participates in the healing of the skin and modulates the inflammatory response.
The cutaneous microbiota would also be able to act on T lymphocytes, to allow them to produce pro-inflammatory cytokines. But this does not only have advantages, this production would be at the origin of pathologies such as psoriasis. The microbiota also participates in the education of antigen-presenting cells, to improve the immune system.
MICROBIOTA, A MAJOR CHALLENGE FOR COSMETICS

Today, the global skin microbiota market in cosmetic care is estimated at $700 million. It is expected to reach 1,950 million by 2029. The word “microbiota” is particularly trendy, since searches for this term on search engines have increased by 80% over the past 5 years.
But why such interest in the skin microbiota? In fact, 82% of cosmetics consumers in the world today encounter skin problems. These problems are for 69% of them itching, for 62% redness and for 55% eczema. Also, 71% of adults report having sensitive skin. Acne can also be reduced by regulating the microbiota. In addition, consumers around the world are turning to the use of beauty products as a priority to correct their skin problem, even before consulting a dermatologist.
It is therefore essential today to develop cosmetic products that meet consumer expectations: to have healthy skin and to fight against a large number of current problems. For this, an answer, a protected and balanced skin microbiota. To promote the development of good bacteria and have healthier skin, you have to take care of it. For example, the use of cosmetics containing prebiotics (inanimate probiotics) or postbiotics is recommended. For this, there are prebiotics and postbiotics based on the enrichment of the skin microbiota or targeting antimicrobial peptides. You also have to be careful with the pH of beauty products, since it can throw the microbiome out of balance.